Incidencia de infecciones del torrente sanguíneo asociadas al catéter venoso central en una unidad de cuidados intensivos pediátricos de un instituto de referencia en Perú, 2009 – 2019
DOI:
https://doi.org/10.58597/rpe.v4i1.99Palabras clave:
Infección hospitalaria, Infecciones Asociadas con Catéteres, Unidades de Cuidado Intensivo Pediátrico, Pediatría, Estudios Longitudinales, PerúResumen
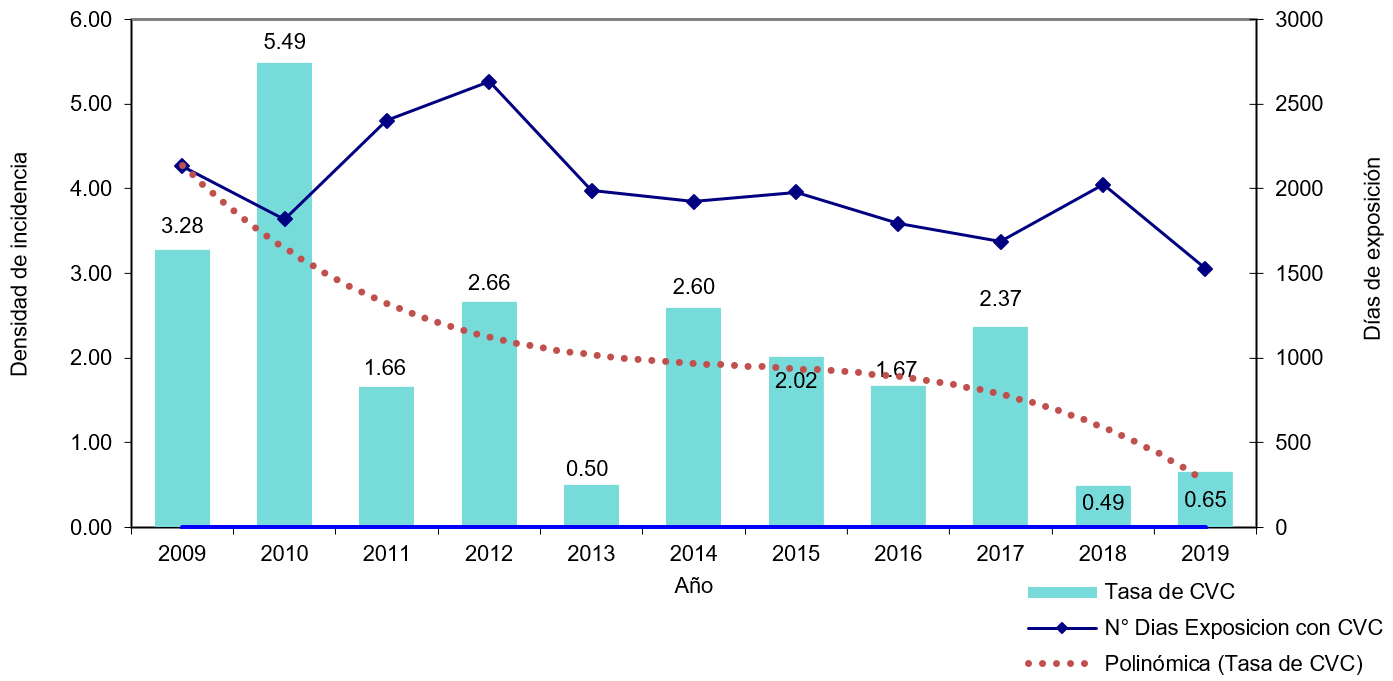
Objetivo: Determinar la incidencia de las infecciones del torrente sanguíneo asociadas a la colocación de catéteres venosos centrales (ITS-CVCs) en la Unidad de Cuidados Intensivos Pediátricos (UCIP) del Instituto Nacional de Salud del Niño (INSN) de Lima, Perú, del 2009 al 2019. Materiales y métodos: Estudio analítico longitudinal retrospectivo que evaluó pacientes menores de 18 años con CVC. Se calcularon las tasas de incidencia de ITS por 1000 días-catéter. Resultados: Se insertaron CVC a 2269 pacientes; 47 pacientes presentaron ITS. La densidad de incidencia promedio de ITS fue de 2,14 por 1000 días-catéter, siendo el pico máximo en el 2010 con 5,49 por 1000 días-catéter. Conclusiones: Hubo una tendencia decreciente de las ITS-CVCs por año. Es necesario seguir con la implementación de protocolos sencillas de costo bajo basadas en evidencia centralizadas y el trabajo multidisciplinario supervisado.
Descargas
Referencias
World Health Organization [Internet]. Report on the Burden of Endemic Health Care-Associated Infection Worldwide. 2011[citado 01 de marzo de 2025]. Disponible en: https://www.who.int/publications/i/item/report-on-the-burden-of-endemic-health-care-associated-infection-worldwide
Allegranzi B, Nejad SB, Combescure C, Graafsman W, Attar H, Donaldson L, et al. Burden of endemic health-care associated infection indeveloping countries: Sistematic review and meta-analysis. Lancet. 2011; 377(9761):228-241. doi:10.1016/S0140-6736(10)61458-4.
Goldstein B, Giroir B, Randolph A; International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6(1):2-8. doi: 10.1097/01.PCC.0000149131.72248.E6.
Melaku EE, Urgie BM, Dessie F, Seid A, Abebe Z, Tefera AS. Determinants of Mortality of Patients Admitted to the Intensive Care Unit at Debre Berhan Comprehensive Specialized Hospital: A Retrospective Cohort Study. Patient Relat Outcome Meas. 2024;15:61-70. doi: 10.2147/PROM.S450502.
Cai Y, Zhu M, Sun W, Cao X, Wu H. Study on the cost attributable to central venous catheter-related bloodstream infection and its influencing factors in a tertiary hospital in China. Health Qual Life Outcomes. 2018;16(1):198. doi: 10.1186/s12955-018-1027-3.
Nakamura I, Fukushima S, Hayakawa T, Sekiya K, Matsumoto T. The additional costs of catheter-related bloodstream infections in intensive care units. Am J Infect Control. 2015;43(10):1046-9. doi: 10.1016/j.ajic.2015.05.022.
Elnasser Z, Obeidat H, Amarin Z. Device-related infections in a pediatric intensive care unit: The Jordan University of Science and Technology experience. Medicine (Baltimore). 2021;100(43):e27651. doi: 10.1097/MD.0000000000027651.
Moro ML, Viganò EF, Cozzi Lepri A. Risk factors for central venous catheter-related infections in surgical and intensive care units. The Central Venous Catheter-Related Infections Study Group. Infect Control Hosp Epidemiol. 1994;15(4 Pt 1):253-64. Disponible en: https://pubmed.ncbi.nlm.nih.gov/8207192/.
Cabrera DM, Cuba FK, Hernández R, Prevost-Ruiz Y. Incidencia y factores de riesgo de infecciones del torrente sanguíneo relacionadas con catéteres de vía central. Rev Peru Med Exp Salud Publica.2021;38(1):95-100. Doi: 10.17843/rpmesp.2021.381.5108
Pittet D, Tarara D, Wenzel RP. Nosocomial bloodstream infection in critically ill patients. Excess length of stay, extra costs, and attributable mortality. JAMA. 1994;271(20):1598-601. doi: 10.1001/jama.271.20.1598.
Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA. 2009;302(21):2323-9. doi: 10.1001/jama.2009.
Nagao M. A multicentre analysis of epidemiology of the nosocomial bloodstream infections in Japanese university hospitals. Clin Microbiol Infect. 2013;19(9):852-8. doi: 10.1111/1469-0691.12083.
Kepenekli E, Soysal A, Yalindag-Ozturk N, Ozgur O, Ozcan I, Devrim I, et al. Healthcare-Associated Infections in Pediatric Intensive Care Units in Turkey: a National Point-Prevalence Survey. Jpn J Infect Dis. 2015;68(5):381-6. doi: 10.7883/yoken.JJID.2014.385.
Nakachi-Morimoto G, Alvarado-Palacios M, Santiago-Abal M, Shimabuku-Azato R. Disminución de las infecciones asociadas al catéter venoso central mediante intervenciones sencillas y de bajo costo, en una unidad de cuidados intensivos pediátricos. An Fac Med. 2017;78(3):303-308. doi: 10.15381/anales.v78i3.13764.
Instituto Nacional de Salud del Niño [Internet]. Plan Operativo Institucional 2024. Minsa. 2024 [citado 01 de marzo de 2025]. Perú. Disponible en: https://www.gob.pe/institucion/insn/colecciones/29153-plan-operativo-institucional-insn
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16(3):128-40. doi: 10.1016/0196-6553(88)90053-3.
Miller MR, Niedner MF, Huskins WC, Colantuoni E, Yenokyan G, Moss M, et al. Reducing PICU central line-associated bloodstream infections: 3-year results. Pediatrics. 2011;128(5):e1077-83. doi: 10.1542/peds.2010-3675.
Furuya EY, Dick A, Perencevich EN, Pogorzelska M, Goldmann D, Stone PW. Central line bundle implementation in US intensive care units and impact on bloodstream infections. PLoS One. 2011;6(1):e15452. doi: 10.1371/journal.pone.0015452.
Edwards JD, Herzig CT, Liu H, Pogorzelska-Maziarz M, Zachariah P, Dick AW, et al. Central line-associated blood stream infections in pediatric intensive care units: Longitudinal trends and compliance with bundle strategies. Am J Infect Control. 2015;43(5):489-93. doi: 10.1016/j.ajic.2015.01.006.
Khieosanuk K, Fupinwong S, Tosilakul A, Sricharoen N, Sudjaritruk T. Incidence rate and risk factors of central line-associated bloodstream infections among neonates and children admitted to a tertiary care university hospital. Am J Infect Control. 2022;50(1):105-107. doi: 10.1016/j.ajic.2021.07.016.
Broudic M, Bodet LM, Dumont R, Joram N, Jacqmarcq O, Caillon J, et al. A 1-year survey of catheter-related infections in a pediatric university hospital: A prospective study. Arch Pediatr. 2020;27(2):79-86. doi: 10.1016/j.arcped.2019.11.004.
Paioni P, Kuhn S, Strässle Y, Seifert B, Berger C. Risk factors for central line-associated bloodstream infections in children with tunneled central venous catheters. Am J Infect Control. 2020;48(1):33-39. doi: 10.1016/j.ajic.2019.06.027.
Moon HM, Kim S, Yun KW, Kim HY, Jung SE, Choi EH, et al. Clinical Characteristics and Risk Factors of Long-term Central Venous Catheter-associated Bloodstream Infections in Children. Pediatr Infect Dis J. 2018;37(5):401-406. doi: 10.1097/INF.0000000000001849.
Contreras-Cuellar GA, Leal-Castro AL, Prieto R, Carvajal-Hermida AL. Device-associated infections in a Colombian neonatal intensive care unit. Rev Salud Publica (Bogota). 2007;9(3):439-47. doi: 10.1590/s0124-00642007000300012.
Advani S, Reich NG, Sengupta A, Gosey L, Milstone AM. Central line-associated bloodstream infection in hospitalized children with peripherally inserted central venous catheters: extending risk analyses outside the intensive care unit. Clin Infect Dis. 2011;52(9):1108-1115. doi: 10.1093/cid/cir145.
Krishnaiah A, Soothill J, Wade A, Mok QQ, Ramnarayan P. Central venous catheter-associated bloodstream infections in a pediatric intensive care unit: effect of the location of catheter insertion. Pediatr Crit Care Med. 2012;13(3):e176-80. doi: 10.1097/PCC.0b013e3182389548.
Sellamuthu R, Nair S, Chandrasekar J, Kesavan S, Shivam V. Risk Factors of Central Line-Associated Bloodstream Infection (CLABSI): A Prospective Study From a Paediatric Intensive Care Unit in South India. Cureus. 2023;15(8):e43349. doi: 10.7759/cureus.43349.
Suresh GK, Edwards WH. Central line-associated bloodstream infections in neonatal intensive care: changing the mental model from inevitability to preventability. Am J Perinatol. 2012;29(1):57-64. doi: 10.1055/s-0031-1286182.
Miller MR, Griswold M, Harris JM 2nd, Yenokyan G, Huskins WC, et al. Decreasing PICU catheter-associated bloodstream infections: NACHRI's quality transformation efforts. Pediatrics. 2010;125(2):206-13. doi: 10.1542/peds.2009-1382.
Randolph AG, Brun-Buisson C, Goldmann D. Identification of central venous catheter-related infections in infants and children. Pediatr Crit Care Med. 2005;6(3 Suppl):S19-24. doi: 10.1097/01.PCC.0000161575.14769.93.
Publicado
Número
Sección
Licencia
Derechos de autor 2025 Graciela Nakachi-Morimoto, Roberto Luis Shimabuku-Azato, Margarita Carmela Alvarado-Palacios

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.