Risk factors for lower respiratory tract infection by Respiratory Syncytial Virus among children under 2 years of age in a hospital in Venezuela
DOI:
https://doi.org/10.58597/rpe.v4i2.102Keywords:
Respiratory Syncytial Virus, Infections, Breastfeeding, Family Medical History, SeasonsAbstract
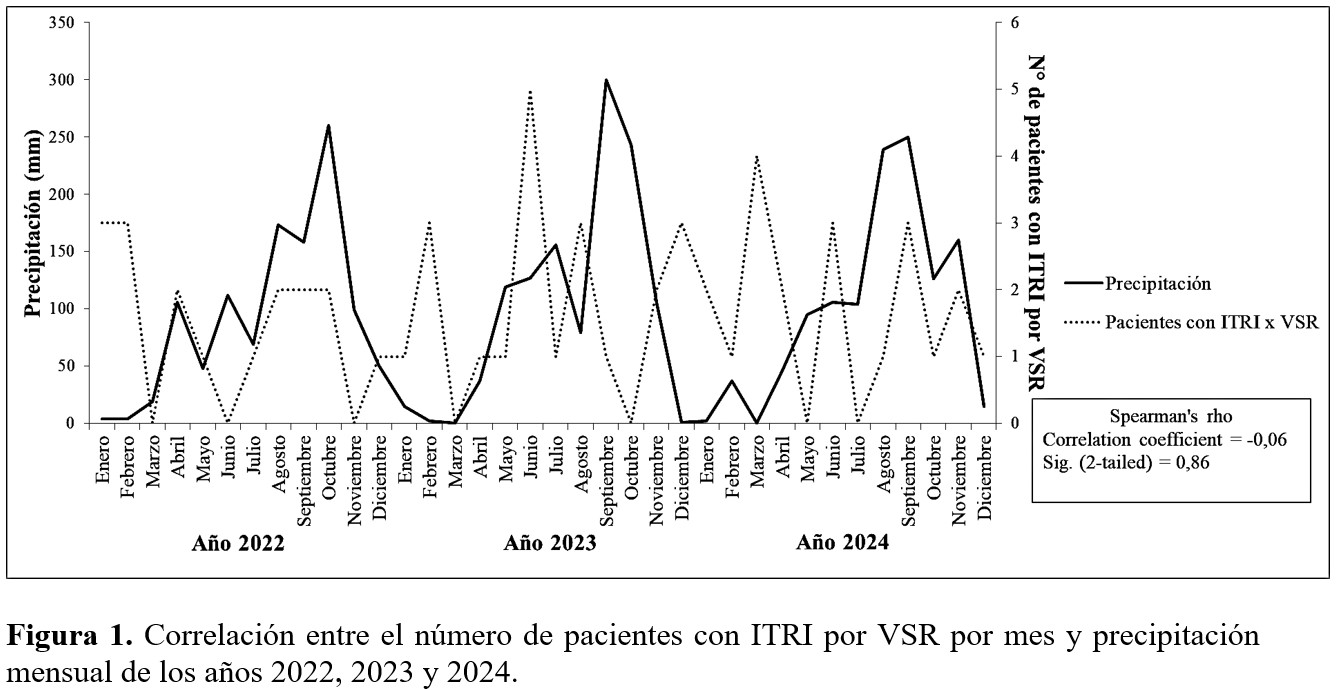
Objective: To identify risk factors for lower respiratory tract infection (LRTI) associated with respiratory syncytial virus (RSV) in children under 2 years of age in a hospital in Venezuela. Materials and methods: A prospective case-control study carried out at the “Santa Cruz” Clinic (Barquisimeto, Lara State, Venezuela), between January 2022 and December 2024, in which 58 cases with LRTI by RSV were compared with 116 controls with LRTI negative for RSV in children under 2 years of age. The number of monthly cases was related to monthly precipitation in the years of the study. In univariate and bivariate analysis, descriptive and inferential statistics were produced by using Spearman’s correlation, Pearson’s ꭓ2, Mann-Whitney U test and binary logistic regression. Results: Factors significantly associated with LRTI by RSV were prematurity, lack of breastfeeding, daycare attendance and family history of asthma. Identified risk factors for LRTI by RSV were lack of breastfeeding (OR=3,94; CI95%: 1,07 – 14,54; p = 0,04), and family history of asthma (OR=2,89; CI95%: 1,20 – 6,97; p = 0,02). There was no significant correlation between the number of monthly cases with monthly precipitation (r = –0,06; p = 0,86). Conclusion: Lack of breastfeeding and family history of asthma were identified as risk factors for LRTI by RSV. No correlation was determined between the number of monthly cases of LRTI by RSV and monthly precipitation.
Downloads
References
Li Y, Wang X, Blau DM, Caballero MT, Feikin DR, Gill CJ, et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in children younger than 5 years in 2019: a systematic analysis. Lancet. 2022; 399: 2047–2064. doi: 10.1016/S0140-6736(22)00478-0
Malo-Sánchez DC. Estacionalidad y severidad de las temporadas de infección respiratoria aguda por Virus Sincitial Respiratorio en Colombia, 2009 a 2016. Reporte Epidemiológico Nacional. [Internet]. 2021; 3(1): 54 - 65. https://doi.org/10.33610/01229907.2021v3n1a4
Deng Sh, Cong B, Edgoose M, De Wit F, Nair H, Li Y. Risk factors for respiratory syncytial virus-associated acute lower respiratory infection in children under 5 years: An updated systematic review and meta-analysis. International Journal of Infectious Diseases. 2024; 146: 107125
Crow R, Mutyara K, Agustian D, Kartasasmita CB, Simões EAF. Risk Factors for Respiratory Syncytial Virus Lower Respiratory Tract Infections: Evidence from an Indonesian Cohort. Viruses. 2021; 13(2): 331. https://doi.org/10.3390/v13020331
Cai W, Buda S, Schuler E, Hirve S, Zhang W, Haas W. Risk factors for hospitalized respiratory syncytial virus disease and its severe outcomes. Influenza Other Respi Viruses. 2020; 00:1–13. https://doi.org/10.1111/ irv.12729
Castro J, Atiencia J, Juma M, Neira V. Estudio Transversal: Prevalencia de Infecciones por Virus Sincitial Respiratorio en Pacientes Ingresados en el Hospital José Carrasco Arteaga, 2017. Rev Med HJCA. 2019; 11(2): 132-136. doi: http://dx.doi.org/10.14410/2019.11.2.ao.21
Departamento de Ingeniería Hidrometeorológica. Facultad de Ingeniería. Escuela de Ingeniería civil. Climatología. Universidad Central de Venezuela. Obtenido de: https://hidromet-ucv.org.ve/category/climatologia
McConnochie K. Bronchiolitis. What´s in the name? Am J Dis Child. 1983; 173:3 – 11.
Pocket Book of Hospital Care for Children: Guidelines for the Management of Common Illnesses with Limited Resources. 2nd ed. World Health Organization, 2013.
World Health Organization Pneumonia Vaccine Trial Investigators Group. Standardization of interpretation chest radiographs for the diagnosis of pneumonia in children. Geneva: World Health Organization; 2001.
CSTE. Revision to the case definition for national pertussis surveillance. CSTE position statement 19-ID-08: Atlanta, GA: CSTE; 2019. Disponible en: https://cdn.ymaws.com/www.cste.org/resource/resmgr/2019ps/final/19-ID-08_Pertussis_final_7.3.pdf
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159-174.
Consenso de la Sociedad Latinoamericana de Infectología Pediátrica (SLIPE). Virus sincitial en América Latina y El Caribe. Revisión de la literatura y Perspectiva regional. 2024. Disponible en: https://slipe.org/web/wp-content/uploads/2024/01/SLIPE-GUIA-VRS-2024.pdf
Goya S, Lucion MF, Shilts MH, Juárez MDV, Gentile A, Mistchenko AS, Viegas M, Das SR. Evolutionary dynamics of respiratory syncytial virus in Buenos Aires: Viral diversity, migration, and subgroup replacement. Virus Evol. 2023; 9(1): vead006. doi: 10.1093/ve/vead006. PMID: 36880065; PMCID: PMC9985318.O
Mena R, Mendoza E, Cabrera De La Cruz J, Calderón M, Maeva Paulino MP, Peguero D. Prevalencia, coinfecciones y circulación estacional del virus sincitial respiratorio (VSR) en pacientes pediátricos de un centro médico en Santo Domingo, República Dominicana. ADOPA. 2023; 1(2): 55-69. I
Chirinos-Saire Y, Reyna-García R, Aguilar-Huauya E, Santillán-Salas C. Virus respiratorios y características clínico-epidemiológicas en los episodios de infección respiratoria aguda. Rev. perú. med. exp. salud pública. 2021; 38(1): 101-107.
Hamid S, Winn A, Parikh R, Jones JM, McMorrow M, Prill MM, et al. Seasonality of Respiratory Syncytial Virus - United States, 2017-2023. MMWR Morb Mortal Wkly Rep. 2023; 72(14):355-61 doi:10.15585/mmwr.mm7214a1.
Shi T, Balsells E, Wastnedge E, Singleton Z, Rasmussen H, Zar B, et al. Nair Risk factors for respiratory syncytial virus associated with acute lower respiratory infection in children under five years: systematic review and meta-analysis. J. Glob. Health. 2015; 5: 10.7189/jogh.05.020416
Shi T, Vennard S, Mahdy S, Nair H, investigators R. Risk Factors for Poor Outcome or Death in Young Children With Respiratory Syncytial Virus-Associated Acute Lower Respiratory Tract Infection: A Systematic Review and Meta-Analysis. J Infect Dis. 2022; 226 (Suppl 1): S10-S6 doi:10.1093/infdis/jiaa751
Rodríguez H, Castro M, Fernández S, Brito E, Pérez M, Urdaneta E, et al. Factores de riesgo para infeccion por virus sincicial respiratorio en Venezuela. Reunion de expertos. Octubre 2013. Archivos Venezolanos de Puericultura y Pediatría. 2016; 79(2): 77-84.
Servadio M, Finocchietti M, Vassallo C, Cipelli R, Heiman F, Di Lucchio G, et al. An epidemiological investigation of high-risk infants for Respiratory Syncytial Virus infections: a retrospective cohort study. Ital J Pediatr. 2024; 50: 56. https://doi.org/10.1186/s13052-024-01627-8
Mineva GM, Purtill H, Dunne CP, Philip RK. Impact of breastfeeding on the incidence and severity of respiratory syncytial virus (RSV)-associated acute lower respiratory infections in infants: a systematic review highlighting the global relevance of primary prevention. BMJ Glob Health. 2023; 8(2): e009693. doi: 10.1136/bmjgh-2022-009693. PMID: 36746518; PMCID: PMC9906265.
Jang MJ, Kim YJ, Hong S, Na J, Hwang J, Shin SM, et al. Positive association of breastfeeding on respiratory syncytial virus infection in hospitalized infants: a multicenter retrospective study. Clin Exp Pediatr. 2020; 63:135–40. 10.3345/kjp.2019.00402
Munblit D, Verhasselt V. Allergy prevention by breastfeeding: possible mechanisms and evidence from human cohorts. Curr Opin Allergy Clin Immunol. 2016; 16:427–33. 10.1097/ACI.0000000000000303
Cacho F, Gebretsadik T, Anderson LJ, Chappell JD, Rosas-Salazar C, Ortiz JR, et al. Respiratory Syncytial Virus Prevalence and Risk Factors among Healthy Term Infants, United States. Emerg Infect Dis. 2024; 30(10): 2199-2202. https://doi.org/10.3201/eid3010.240609
Martín A, Martín J, Martín M. La guardería. Pediatr Integral. 2019; 23 (2): 110.e1 – 110.e9
Figueras-Aloy J, Carbonell-Estrany X, Quero-Jiménez J, et al; IRIS Study Group. FLIP-2 Study: risk factors linked to respiratory syncytial virus infection requiring hospitalization in premature infants born in Spain at a gestational age of 32 to 35 weeks. Pediatr Infect Dis J. 2008; 27: 788-93.
Divarathna V, Rafeek M, Morel J, Aththanayake Ch, Noordeen Faseeha. Epidemiology and risk factors of respiratory syncytial virus associated acute respiratory tract infection in hospitalized children younger than 5 years from Sri Lanka. Front. Microbiol. 2023; 14: DOI=10.3389/fmicb.2023.1173842
Stamataki S, Georgountzou A, Papadopoulos NG, Taka S, Maggina P, Xepapadaki P, Prokopakis E. Atopic children are more susceptible to viral respiratory infection at the age of 2-5 years old. Allergy Asthma Proc. 2023; 44(1): 64-70. doi: 10.2500/aap.2023.44.220092.
Puma-Olguin TC, Mazagatos C, Galindo-Carretero S, Vega-Piris L, Lozano-Álvarez M, Pérez-Gimeno G. et al. Epidemiología y carga de enfermedad por VRS en España. SiVIRA, temporadas 2021-22 y 2022-23. Boletín EpidemiológicoSemanal. 2024; 32(1):21-35. doi: 10.4321/s2173-92772024000100003
Gentile A, Lucion M, Juarez M, Areso M, Bakir J, et al. Burden of respiratory syncytial virus disease and mortality risk factors in Argentina: 18 years of active surveillance in a children's hospital. Pediatric Infectious Disease Journal. 2019; 38 (6): 589-594
Downloads
Additional Files
Published
Issue
Section
License
Copyright (c) 2025 Omar E. Naveda-Romero, Rafael j. Meléndez-Freitez, Anyerly J. Reaño-Alvarado

This work is licensed under a Creative Commons Attribution 4.0 International License.