Long-term survival of patients with postoperative complications in cardiac surgery: Experience of a specialized pediatric institute in Peru, 2001-2019
DOI:
https://doi.org/10.58597/rpe.v3i4.94Keywords:
Thoracic Surgery, Cardiopulmonary Bypass, Postoperative ComplicationAbstract
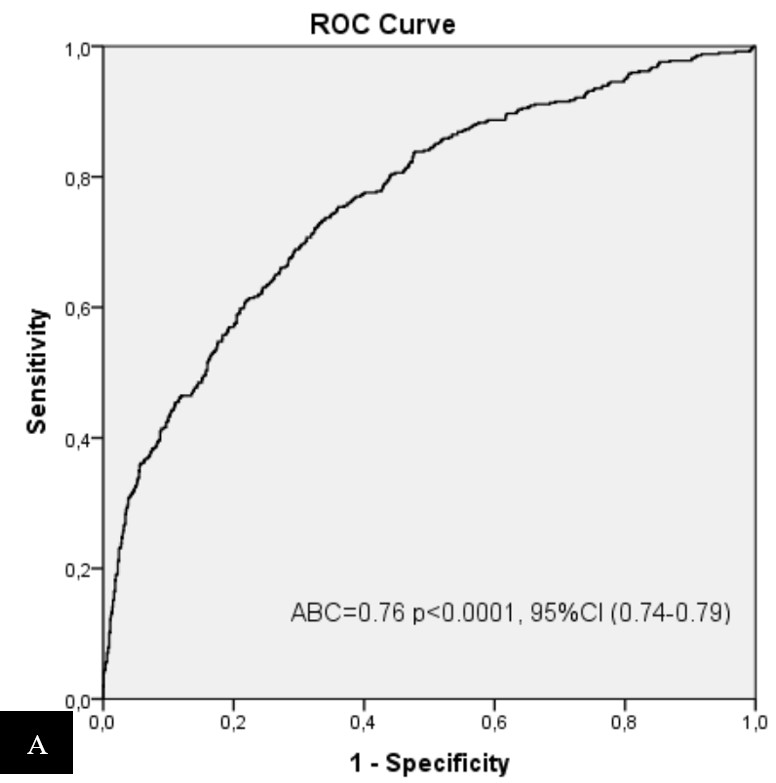
Objective: To evaluate the impact of complications on short- and long-term survival after cardiac surgery. Materials and methods: Retrospective cohort of patients after their first cardiac surgery at the Instituto Nacional de Salud del Niño from 2001 to 2019. A multivariate and Cox regression analysis identified predictors of early and late complications and mortality. Results: 1709 children were included and the overall rate of major complications was 29.3%; being 20% cardiac and 17.1% extracardiac. Overall mortality was 11.9%, with operative mortality (30 days or before hospital discharge) being 6.4% and 8.9% at one year. A higher number of complications affected operative (p < 0.0001), 90-day (p < 0.0001), 120-day (p < 0.0001) and 1-year (p < 0.0001) mortality. Reoperation (HR = 2.3; 95 % CI: 1.6-3.4), low cardiac output (HR = 8.5; 95 % CI: 6.0-12.0), cardiac arrest (HR = 7.7; 95 % CI: 4.3-13.6), sepsis (HR = 8.1; 95 % CI: 5.8-11.5) and peritoneal dialysis (HR = 3.7; 95 % CI: 2.3-6.2) were associated with higher 1-year mortality. Conclusions: There is a strong association between the type and number of postoperative complications with decreased early and long-term survival. It is justified to identify and control risk factors in early stages.
Downloads
References
Cameron D. Initiation of white cell activation during cardiopulmonary bypass: cytokines and receptors. J Cardiovasc Pharmacol. 1996;27 Suppl 1:S1-S5. doi:10.1097/00005344-199600001-00004.
Futterman C, Salvin JW, McManus M, et al. Inadequate oxygen delivery index dose is associated with cardiac arrest risk in neonates following cardiopulmonary bypass surgery. Resuscitation. 2019; 142:74-80. doi: 10.1016/j.resuscitation.2019.07.013
Agarwal HS, Wolfram KB, Saville BR, Donahue BS, Bichell DP. Postoperative complications and association with outcomes in pediatric cardiac surgery. J Thorac Cardiovasc Surg. 2014;148(2):609-16. e1. doi: 10.1016/j.jtcvs.2013.10.031.
Murni IK, Djer MM, Yanuarso PB, et al. Outcome of pediatric cardiac surgery and predictors of major complication in a developing country. Ann Pediatr Cardiol. 2019;12(1):38-44. doi: 10.4103/apc.APC_146_17.
Belliveau D, Burton HJ, O'Blenes SB, Warren AE, Hancock Friesen CL. Real-time complication monitoring in pediatric cardiac surgery. Ann Thorac Surg. 2012;94(5):1596-1602. doi: 10.1016/j.athoracsur.2012.05.103.
Roodpeyma S, Hekmat M, Dordkhar M, Rafieyian S, Hashemi A. A prospective observational study of pediatric cardiac surgery outcomes in a postoperative intensive care unit in Iran. J Pak Med Assoc. 2013;63(1):55-59. Disponible en: https://pubmed.ncbi.nlm.nih.gov/23865132/
Kumar SR, Gaynor JW, Heuerman H, et al. The Society of Thoracic Surgeons Congenital Heart Surgery Database: 2023 Update on Outcomes and Research. Ann Thorac Surg. 2024;117(5):904-914. doi: 10.1016/j.athoracsur.2024.03.018
Seese L, Sultan I, Gleason TG, et al. The Impact of Major Postoperative Complications on Long-Term Survival After Cardiac Surgery. Ann Thorac Surg. 2020;110(1):128-135. doi : 10.1016/j.athoracsur.2019.09.100.
Pasquali SK, Li JS, Burstein DS, et al. Association of center volume with mortality and complications in pediatric heart surgery. Pediatrics. 2012;129(2): e370-e376. doi:10.1542/peds.2011-1188.
Gaies M, Pasquali SK, Donohue JE, et al. Seminal Postoperative Complications and Mode of Death After Pediatric Cardiac Surgical Procedures. Ann Thorac Surg. 2016;102(2):628-635. doi: 10.1016/j.athoracsur.2016.02.043.
Costello JM, Preze E, Nguyen N, et al. Experience with an Acuity Adaptable Care Model for Pediatric Cardiac Surgery. World J Pediatr Congenital Heart Surg. 2017;8(6):665-671. doi:10.1177/2150135117733722.
Brown KL, Ridout D, Pagel C, et al. Incidence and risk factors for important early morbidities associated with pediatric cardiac surgery in a UK population. J Thorac Cardiovasc Surg. 2019;158(4):1185-1196.e7. doi: 10.1016/j.jtcvs.2019.03.139.
Althabe M, Rodríguez R R, Balestrini M, et al. Morbidity in congenital heart surgery in a public hospital in Argentina. Arch Argent Pediatr. 2018 ;116(1):e14 -e18. doi: 10.5546/aap.2018.eng.e.
Javed F, Aleysae NA, Al- Mahbosh AY, et al. Complications After Surgical Repair of Congenital Heart Disease in Infants. An Experience from Tertiary Care Center. J Saudi Heart Assoc. 2021;33(4):271-278. Published 2021 Oct 15. doi:10.37616/2212-5043.1267.
Jacobs ML, O'Brien SM, Jacobs JP, et al. An empirically based tool for analyzing morbidity associated with operations for congenital heart disease. J Thorac Cardiovasc Surg 2013;145:1046–57. doi: 10.1016/j.jtcvs.2012.06.029.
Zeng X, An J, Lin R, et al. Prediction of complications after pediatric cardiac surgery. Eur J Cardiothorac Surg. 2020;57(2):350-358. doi:10.1093/ ejcts /ezz198.
Shi S, Xiong C, Bie D, Li Y, Wang J. Development and Validation of a Nomogram for Predicting Acute Kidney Injury in Pediatric Patients Undergoing Cardiac Surgery. Pediatrician Cardiol. 2024. doi:10.1007/s00246-023-03392-7.
Kim WH, Ji SH, Jang YE. Can machine learning-based prediction of complications after pediatric cardiac surgery improve patient outcomes? Eur J Cardiothorac Surg. 2020;58(2):400. doi:10.1093/ ejcts /ezaa086.
Mayer JE Jr, Hill K, Jacobs JP, Overman DM, Kumar SR. The Society of Thoracic Surgeons Congenital Heart Surgery Database: 2020 Update on Outcomes and Research. Ann Thorac Surg. 2020;110(6):1809-1818. doi: 10.1016/j.athoracsur.2020.10.004.
Furlong-Dillard J, Bailly D, Amula V, Wilkes J, Bratton S. Resource Use and Morbidities in Pediatric Cardiac Surgery Patients with Genetic Conditions. J Pediatr. 2018; 193:139-146.e1. doi: 10.1016/j.jpeds.2017.09.085.
Ross F, Latham G, Joffe D, et al. Preoperative malnutrition is associated with increased mortality and adverse outcomes after pediatric cardiac surgery. Cardiol Young. 2017;27(9):1716-1725. doi:10.1017/S1047951117001068.
Griffeth EM, Stephens EH, Burchill LJ, et al. Risk of Cardiac Reoperation: An Analysis of The STS Congenital Heart Surgery Database. Ann Thorac Surg. Published online June 25, 2024. doi: 10.1016/j.athoracsur.2024.06.013.
Wang P, Fu C, Bai G, et al. Risk factors of postoperative low cardiac output syndrome in children with congenital heart disease: A systematic review and meta-analysis. Front Pediatr. 2023; 10:954427. doi:10.3389/fped.2022.954427.
Du X, Chen H, Song X, et al. Risk factors for low cardiac output syndrome in children with congenital heart disease undergoing cardiac surgery: a retrospective cohort study. BMC Pediatr. 2020;20(1):87. doi:10.1186/s12887-020-1972-y.
Shahzad M, Alheraish YA, Algethami B, et al. Original Article--Risk Factors for Neurological Complications and Short-term Outcomes After Pediatric Heart Surgery: A Retrospective Analysis. J Saudi Heart Assoc. 2024;36(1):8-13. Published 2024 Mar 3. doi:10.37616/2212-5043.1364.
Wasniewski ABR, Ricachinevsky CP, Rezende RQ, et al. Adverse events in the postoperative period of cardiac surgery in a pediatric intensive care unit: the contribution of the VIS score and the RACHS-1. Crit Care Sci. 2023;35(4):377-385. doi:10.5935/2965-2774.20230215-en.
Simsek B, Ozyuksel A, Saygi M, Bilal MS. Plication for diaphragm paralysis after pediatric cardiac surgery: a single- center experience. Cardiol Young. 2023;33(10):2087-2093. doi:10.1017/S1047951123000276.
Samanidis G, Kourelis G, Bounta S, Kanakis M. Postoperative Chylothorax in Neonates and Infants after Congenital Heart Disease Surgery-Current Aspects in Diagnosis and Treatment. Nutrients. 2022;14(9):1803. doi:10.3390/nu14091803.
Neumayr TM, Alge JL, Afonso NS, Akcan- Arikan A. Acute Kidney Injury After Pediatric Cardiac Surgery. Pediatr Crit Care Med. 2022;23(5):e249-e256. doi:10.1097/PCC.0000000000002933.
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Luis Eduardo Silva-Delgado, Alfredo Jáuregui-Farfán, Carlos Espiche-Salazar, Piero Larco-Castilla, Rocío Dávalos-Quevedo, Katherine Silva-Delgado, Eduardo Wilfredo Silva-Rivera

This work is licensed under a Creative Commons Attribution 4.0 International License.